Beyond Bias
Reducing healthcare provider bias that hinders the provision of contraceptive information and services to adolescents
Project:
Beyond Bias
Location:
Pakistan, Burkina Faso, Tanzania
Funders:
Bill and Melinda Gates Foundation
Partners:
Pathfinder International, Camber Collective, BERI
Category:
Sexual & Reproductive Health
Challenge
There is a global unmet need for contraception.
Of the estimated 38 million sexually active adolescents ages 15-19 in developing regions who don’t want a child in the next two years, 23 million have an unmet need for contraception. Adolescents have low use of long-acting reversible contraception (LARC) suggesting they are not consistently offered a full choice of contraceptive methods. Among adolescent women in developing regions who use modern contraceptives, only 5% use intrauterine devices (IUDs) and 8% use implants. There are many factors that contribute to low usage of contraception among adolescents, including but not limited to community stigma, low knowledge, and misconceptions about side effects.
One of the persistent and pervasive barriers that hinders young people from accessing sexual & reproductive health services is judgment and bias from the healthcare provider when they try to seek services. We call this provider bias “the last meter of care challenge.” After all, a young person can’t begin using a contraceptive method if their local provider refuses to give it to them.
There has never been a targeted intervention that aims to address provider bias. Most efforts to increase universal access and reduce unintended pregnancy have been focused on improvements to expand access to high-quality services by improving facility settings, training providers on medical standards, and generating demand. Provider bias towards young clients seeking contraception is an entrenched problem that has seen little progress for decades.
Provider bias is a complicated challenge that requires new multidisciplinary thinking. It is influenced by factors including social and gender norms, religious beliefs, local policies, social and demographic characteristics of clients, professional environments, and lack of information, along with a myriad of other factors. It requires a deep understanding of bias, how it differs by circumstance, and how it can be changed.
Beyond Bias was the first project of its kind to rigorously characterize bias across multiple countries and systematically test solution approaches to address provider bias.
Innovation
Beyond Bias is a novel, scalable service model that reduces healthcare providers’ implicit biases and improves treatment outcomes for patients. Our interdisciplinary approach combined traditional adolescent sexual & reproductive health expertise, human-centered design, behavioral economics, social behavior change communication, and segmentation analysis. Over 800 providers and 300 young people were engaged in the research, design, and testing of solution approaches, guided by YLabs’ design process.
The resulting Beyond Bias intervention is a three-pillared program that supports healthcare providers at every phase of their journey from developing awareness of their own bias to becoming advocates for improving contraceptive services for youth in their community.
Although the overall intervention strategy is the same across all three countries in order to increase scalability, we used provider segmentation analysis (produced by Camber Collective) to tailor the program for each of the three countries, in order to increase the likelihood of behavior change impact. The intervention has three key experience phases for providers:
Activate
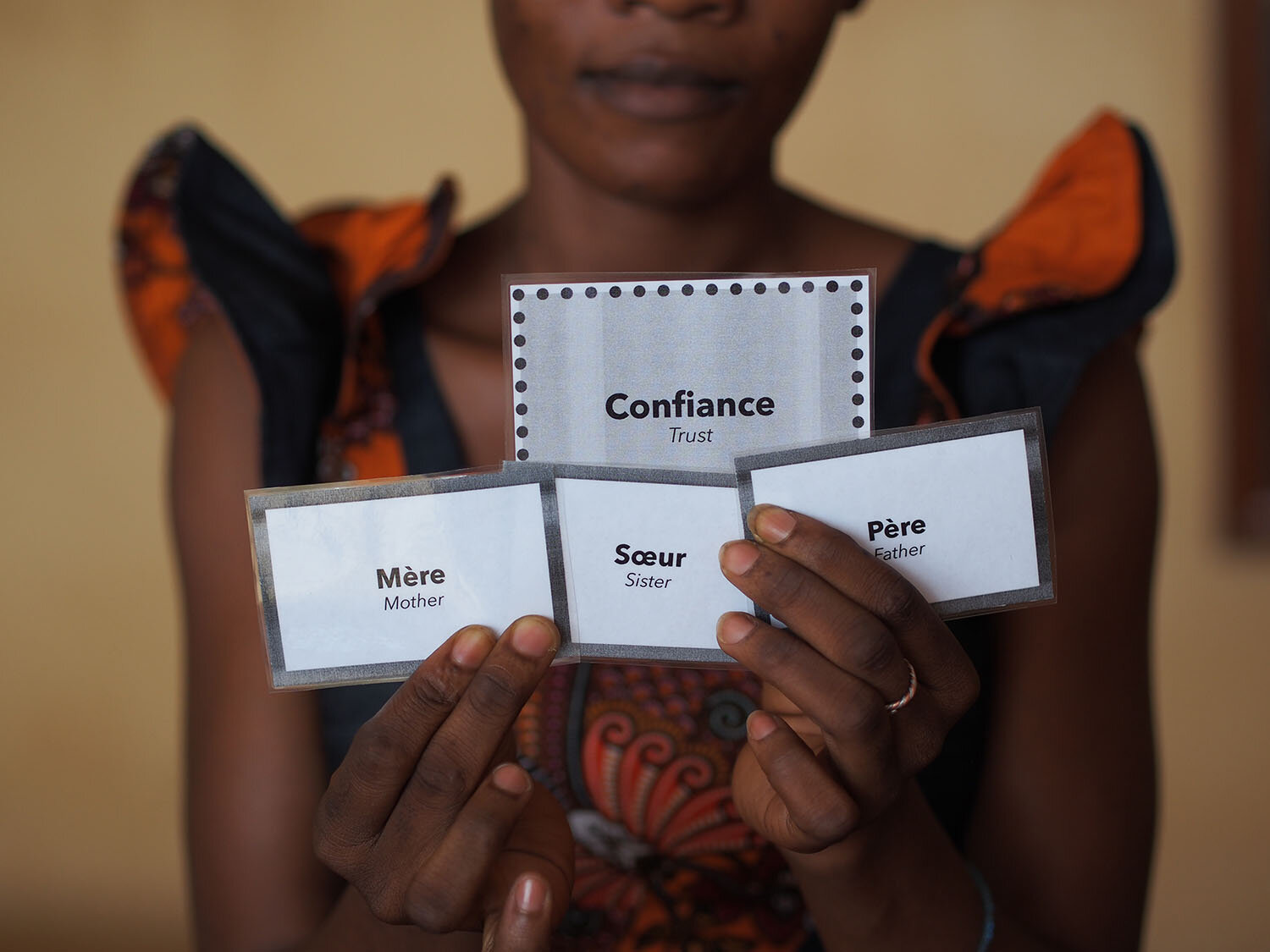
Providers gather for a one-day in-person, story-driven event that activates providers’ self-awareness of their own biases and empathy for their young clients. Through the youth-driven design process and multiple rounds of user testing, we evolved the event to effectively support providers to reflect on their own biases, publicly discuss them, and create an action plan for shifting them alongside their peers.
Apply
After the initial event, providers receive ongoing peer support and learning through WhatsApp groups or regular in-person forums led by their supervisors. In these groups, providers are able to problem-solve together to share how to apply unbiased practices in their daily work and enable providers to support each other when they encounter challenges. Through iterative testing and co-design with providers, we adapted the content to be valuable, relevant, and motivating to providers, rather than simply feeling like “school” or a nagging friend.
Achieve
Each quarter, providers are given feedback on their progress and the opportunity for recognition for their achievements. We designed a growth-oriented performance rewards system based on client feedback. Facilities receive report cards with performance data and recommendations for improvement. As part of the design process, we developed a digital audio-visual client exit survey app to collect client feedback after interacting with a provider. We tested the app with over 3,000 youth clients at 29 facilities across the three countries during the prototyping phase. Through user testing, we were able to refine the app for equitable accessibility; it can be used by young clients with low literacy and low experience with technology.
The Beyond Bias project has produced a variety of outputs that can benefit other organizations or AYSRH practitioners.
Foundational Research:
Camber Collective’s taxonomy of drivers of provider bias and provider segments with different bias profiles
YLabs’ qualitative study of the drivers and consequences of provider bias based on interviews with 311 providers, youth, and community members in the three focus countries
Research Tools:
Provider segmentation tools and screener surveys
Intervention Strategy:
An adaptable behavior change model and design principles for shifting bias across diverse contexts
Next Steps
In September 2019, Beyond Bias began its implementation phase in each of the three focus countries with a total of 233 clinics. A randomized controlled trial (RCT) was conducted to evaluate the project’s impact on provider behavior and attitudes over a period of 12 months.
Survey data from youth client exit interviews and mystery client visits demonstrated that, at the end of the pilot period, youth in Tanzania and Pakistan received more comprehensive sexual and reproductive health counseling and more tailored treatment compared to a control group. Furthermore, providers reported a shift in their own attitudes and behavior toward youth clients, which was demonstrated through more supportive counseling and fewer service refusals.
For more details on the project, methodology, evaluation, and results, read the full project report below. Also, check out our FP2020 webinar in English or in French to hear more about the project and our learnings.